The Best Yeast Infection Treatments for 2023
Vaginal Health: Remedies And Treatments For Vaginal Odor
Some vaginal odors do not need to be addressed at all and are the normal result of healthy bacteria in the vagina and changes in the menstrual cycle.
But when it comes to getting rid of abnormal odors, Cheruba Prabakar, M.D., a board-certified OB-GYN based in Lafayette, California and Luna Daily medical advisor, says identifying the root cause is key.
"If the odor is fishy, that likely signifies a bacterial vaginosis infection that can be treated with antibiotics. Yeast infections can also be treated with medication," says Dr. Prabakar. "These are prescribed by your doctor after an evaluation."
Proper hygiene is another way to get rid of vaginal odor, particularly if it's sweat, hygiene or foreign object-related, Dr. Poucher says. "Shower daily and wash your hands before touching your vagina," she says. "Wear breathable, well-fitting underwear, ideally cotton."
How to Prevent Vaginal OdorIf you want to stop vaginal odor from popping up in the first place, here are some prevention methods to keep in mind.
Shower DailyShowering daily, particularly if you exercise and sweat a lot, can be a helpful way to prevent vaginal odor. But remember, a little warm water is all you need. "Make sure to wash the area from front to back to avoid spreading bacteria from the anus to the vagina," Dr. Chuang says.
Drink Enough WaterHydration can be incredibly helpful when it comes to keeping vaginal odor normal. "Drinking plenty of water helps maintain overall vaginal health by flushing out toxins and promoting proper hydration," says Dr. Chuang.
Eat a Healthy DietLike hydration, eating a healthy diet is important for vaginal health. "A healthy diet rich in fruits, vegetables, whole grains and lean proteins can help support a healthy vaginal environment," says Dr. Chuang. "Avoid excessive consumption of sugary or processed foods, as they can contribute to imbalances in vaginal bacteria."
Avoid Douches and Scented ProductsWhile douches and scented products were once thought to improve the smell of the vagina, experts say they're a bad idea. "There are many suppositories, douches, creams and lotions that promise to 'take away vaginal odor,'" says Dr. Prabakar. "While their promises may seem enticing, it is important to remember that some vaginal odor is normal. When it comes to vaginal health, less is more. Protect your vaginal microbiome."
Avoid Moistened Wipes that Contain AlcoholMoistened wipes that contain alcohol should be avoided when it comes to vaginal health. "Skip moistened wipes that contain alcohol as they will dry the vagina out and create more irritation," says Dr. Poucher.
Wear Breathable UnderwearBreathable underwear are important when it comes to maintaining a balanced pH in the vagina. "Opt for underwear made from natural fabrics like cotton, as they allow for better airflow and help keep the vaginal area dry," suggests Dr. Chuang. "Avoid tight-fitting underwear or synthetic materials that can trap moisture and promote bacterial growth."
Private Party For Your Vaginal Health
A potent probiotic + cranberry supplement to help balance the vaginal microbiome and promote optimal urinary tract function.
Yeast Can Trigger Bowel Inflammation
Inflammatory bowel diseases (IBDs) include Crohn's disease and ulcerative colitis, in which the gastrointestinal tract is chronically inflamed. These disorders can have a significant negative impact on quality of life, and there are few treatment options that help all patients. The causes of these disorders are still under investigation, but it's thought that one reason they happen is because the immune system has an aberrant response to the gut microbiome. But the composition of normal, healthy gut microbiomes can vary considerably from one person to another, and it's been challenging to decipher exactly how the microbiome is involved in IBD. The immune system is extremely complex, and different immune cells may also be related to IBD in different patients. Scientists have now suggested that yeast cells can be a major trigger for IBD.
The gut microbiome is thought to be disrupted in Crohn's disease, in which flares of inflammation occur over and over in patients, who experience diarrhea, cramping, and other symptoms. T cells are likely a major player in Crohn's disease; they carry receptors that react to proteins on microbial cell surfaces, and can trigger immune reactions, or inflammation, in response.
In this study, the investigators wanted to identify the microbes that caused altered T cell responses that are seen in Crohn's disease, said first study author Gabriela Rios Martini, a doctoral candidate in the lab of Professor Petra Bacher at Kiel University (CAU) and the University Hospital Schleswig-Holstein (UKSH). The findings have been reported in Nature Medicine.
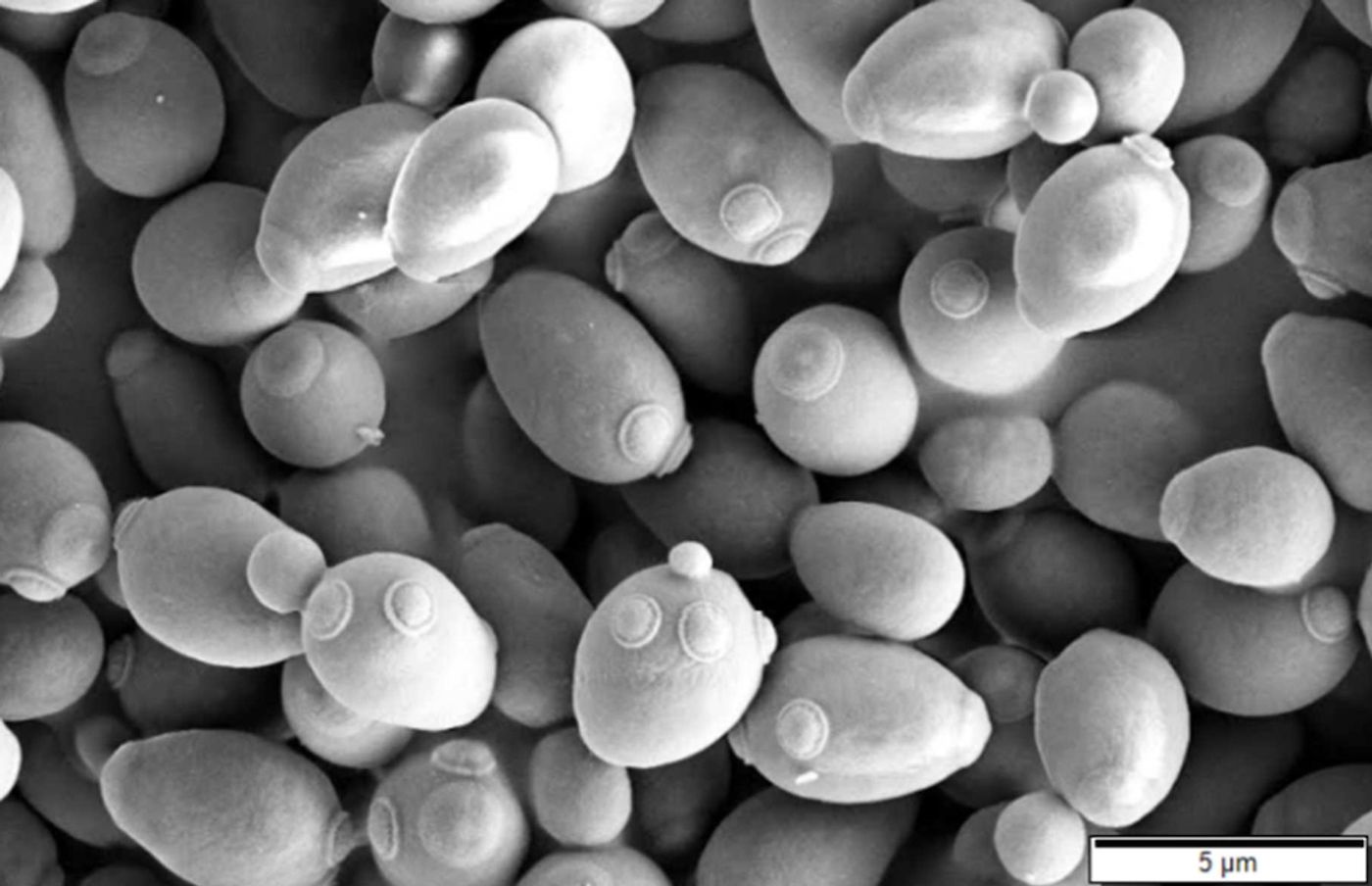
The team assessed how T cells in blood and tissue were responding to certain bacteria in people with and without IBD, and did not find differences. "But then we looked at the T-cell responses to yeast fungi, such as various Candida or Saccharomyces species, and surprisingly found a massively increased T-cell response in Crohn's disease patients," noted Rios Martini.
The investigators analyzed the effects of yeasts that are consumed in food, and those that are a natural part of the healthy human microbiome. They sequenced the genomes of T cells that reacted to yeast, and found that in IBD patients, there were high levels of T cells that can respond to many different types of Candida and Saccharomyces yeast fungi.
"Apparently, the T cells specifically recognize a certain part in these related yeast fungi that is present in many of the species studied," explained senior study author Professor Petra Bacher from the Institute of Immunology and the Institute of Clinical Molecular Biology, CAU and UKSH.
These T cells can react to both broad and specific types of Candida and Saccharomyces, in a phenomenon known as cross-reactivity.
"Overall, our data suggests that after an initial T-cell response against yeast, repeated contact with antigens found in multiple yeasts leads to activation and proliferation of cross-reactive T cells," Bacher explained. "So the immune response is probably triggered again and again, which most likely also contributes to the chronicity of the inflammation."
Both the yeast in the microbiome and yeasts that are ingested in food could play a role in IBD.
This research could open up new treatment options. Now, the scientists want to determine how yeast elimination diets or antifungal therapies could help patients. It may also be possible to disrupt the cross-reactivity.
The study authors noted that yeast fungi have not gotten enough research attention, yet. "For the first time, we have identified strong evidence for the involvement of yeast-reactive T cells in the inflammatory response in Crohn's disease. More research is now needed to determine their direct contribution to the pathophysiology of the disease," said study co-author Professor Stefan Schreiber, Director of the Department of Internal Medicine I, UKSH, Campus Kiel, among other appointments.
Sources: Kiel University, Nature Medicine
Can You Have BV And Yeast Infection At The Same Time? Yes! Ob/Gyns Share The Best At-Home Remedies For Both
If you've ever had a yeast infection (and research shows that 75% of us have), you're all too familiar with the telltale symptoms like itching, burning and discharge. And many women get the pesky infections again and again. But sometimes, those symptoms aren't a sign of a yeast infection at all! Gynecologists are reporting that many women who think they have a yeast infection are self-misdiagnosing a totally different vaginal condition called bacterial vaginosis (BV). Both conditions come with similar uncomfortable symptoms and it can be hard to tell them apart. For that reason, many women are asking, "Can you have BV and a yeast infection at the same time?" The answer is yes. The good news is that it's possible to cure both infections. Read on for the must-know info.
"One of the big misconceptions is every time someone thinks they have vaginal irritation or odor or an abnormal discharge, they think it's yeast, and in fact, most times, it's not," says Lauren Streicher, MD, an associate clinical professor of obstetrics and gynecology at Northwestern University. "Most times, it's bacterial vaginosis, which is an imbalance in the bacteria in the vagina." It's surprisingly common, with research showing that up to 30% of the time women with BV also have yeast overgrowth.
If you're not sure whether you have a yeast infection or bacterial vaginosis (or both, ugh!), doctors agree that it's crucial that you visit the gynecologist to see what's going on. Here, what you need to know about these conditions and how you can get relief.
Yeast infection basicsIt's normal for a yeast called Candida albicans to live in the vagina. But everything from birth control pills and hormone therapy to antibiotics and uncontrolled diabetes can cause the vaginal tract to become more hospitable to the yeast, which then overgrows, leading to symptoms like vaginal discharge, itching and burning during sex or while urinating, says Barbara DePree, MD, a certified menopause practitioner and founder of MiddlesexMD.Com.
Bacterial vaginosis basicsAge-related hormone fluxes, menstruation and even sex can bring a rise in vaginal pH that allows harmful bacteria to flourish, leading to bacterial vaginosis, a condition that causes odor and an itchy, irritating discharge, explains Laura Corio, MD, author of The Change Before The Change. Normally, the vaginal pH is pretty low, between 3.5 to 4.5, which allows the healthy bacteria in your body to thrive. But if something elevates the pH — such as sexual intercourse or the use of lubricants and douches — the "good bacteria" have trouble thriving and the "bad" bacteria start to take over.
How to tell if it's a yeast infection or bacterial vaginosisIf you have a yeast infection, you can expect to see a white, thick vaginal discharge that resembles cottage cheese. You'll probably feel very itchy down there, and you may spot some redness on the vulva and around the opening of the vagina. You may also notice a mild yeasty odor, but it probably won't be too strong of a smell.
Both BV and yeast infections cause burning and itching, but fishy odor and a thin grayish discharge are hallmark signs of BV, says Dr. Corio. And unlike a yeast infection, there does tend to be a strong fish-like odor with bacterial vaginosis. This odor can get even worse after you have intercourse.
To determine which one you have, Dr. Corio recommends seeing your doctor for a vaginal culture test. If the test confirms BV, your doctor can prescribe antibiotics to kill the infection.
If you're prone to repeat yeast infections, you likely keep over-the-counter treatments on hand. But before you use them, Dr. Corio says you might find it helpful to test your vaginal pH using an at-home kit (like AZO Vaginal pH Test Kit, Buy on Amazon, $14.01 for 2 tests). Simply insert the cotton swab in your vagina, then apply to the included pH test pad. A normal pH is 3.5 to 4.5; a pH of 5 or higher is abnormal. "If your vaginal pH is abnormal, you should see a doctor, who can determine the cause and prescribe targeted treatment," advises Dr. Corio.
How to treat BVIf you discover that you do have bacterial vaginosis, your doctor will prescribe antibiotics to treat it. And while antibiotics will kill the bacteria that cause BV, they can also knock out the vagina's healthy flora, leaving you vulnerable to recurrence. Thankfully, these natural options are proven to treat BV and keep future infections at bay:
Spoon up yogurtRoberto Machado Noa/Getty Images
"Since the depletion of good vaginal bacteria (lactobacillus) is the root cause of BV, it makes sense to replenish them," says Dr. DePree. "Studies have shown a 60% reduction in infections in women who eat probiotic-enhanced yogurt daily for 30 days." (Click through for a simple recipe to make your own probiotic yogurt). Don't like yogurt? Dr. DePree advises taking a probiotic with lactobacillus once daily (like Nature's Way Probiotic Pearls for Women, Buy on Amazon, $10.75 for 30).
Try vitamin C this wayInserting a 250-mg. Vitamin C tablet into the vagina for six days in a row cured BV for 86% of women in a study published in the Journal of Clinical Medicine Research. How it works: Vitamin C restores a healthy pH level in the vagina to enhance the body's ability to fight off infectious bacteria. Dr. Corio recommends using an enteric-coated pill to avoid irritation to sensitive vaginal tissue and inserting a tablet twice weekly to prevent future infections.
How to keep BV from returning"There is some scientific evidence that using over-the-counter vaginal probiotic capsules that contain lactobacilli (like VagiBiom, Buy on Amazon, $34.95 for 15 suppositories) can help protect against BV in women with a history of repeat infections — and you don't have to use them every single day," says Dr. DePree. One study found that a pattern of seven days on and seven days off reduced recurrence rates by 65%.
Finally, Dr. DePree notes, consider using hypoallergenic, fragrance-free soap, wearing breathable cotton underwear. You should also avoid douching since it disrupts the vagina's balance of good to bad bacteria, which can trigger an infection.
How to treat a yeast infection Antifungal medicationsAntifungal medications like over-the-counter Monistat (Buy on Amazon, $12.97) and prescription Diflucan can treat yeast infections, but Dr. DePree notes that "certain strains of fungi, such as Candida albicans, the one responsible for most yeast infections, can become resistant to over-the-counter antifungal creams or suppositories.
There's also Vivjoa, a newer prescription oral medication — the first treatment designed to treat repeat yeast infections, or recurrent vulvovaginal candidiasis (RVVC). "This antifungal drug is more effective than current antifungal treatment options because it's less likely to cause antifungal resistance while still killing fungal growth," says Dr. DePree. Although it's not a quick fix (the medication must be taken for three months), 96% of women with RVVC using Vivjoa were free from recurrent infections for nearly a year. (Note: The medication isn't recommended for women who are pregnant or breastfeeding.)
If you prefer natural strategies, consider these:
Vitamin BA form of vitamin B-3 called nicotinamide reduces the number of candida cells by 67% and enhances the power of prescription antifungal drugs, say Chinese researchers. You can get B-3 from foods like eggs, dairy, poultry, fish and enriched grains or by taking a supplement, like Life Extension NAD+ Cell Regenerator (Buy on Amazon, $45 for 30 capsules).
This purple remedyGentian violet (GV) is an antiseptic that prevents candida spores from producing infection-causing proteins, and a 2022 study in the Journal of Obstetrics and Gynaecology found that women who used GV in addition to a prescription antifungal were more likely to cure the infection and did so one day sooner. What's more, their infections were 55% less likely to return. To get the benefits, pour 2 tsp. Of a diluted, 1% solution of GV (like De La Cruz Gentian Violet, buy on Amazon, $9.18 for a 1-oz. Bottle) into a glass, soak a tampon in the solution and wear the tampon for up to 3 hours twice a day for three days. Note: GV stains skin and clothing, so consider using a pad or panty liner to protect your clothes.
Other smart strategies Dr. DePree recommends to help restore healthy vaginal pH levels and protect against future yeast overgrowth: reducing your intake of sugar and refined carbohydrates (yeast's favorite food), avoiding douching and scented vaginal products that can disrupt the microbial balance and supplementing with a daily probiotic. (Click through to learn about the natural yeast infection cure that helped one woman heal and about kombucha for yeast infections)
This content is not a substitute for professional medical advice or diagnosis. Always consult your physician before pursuing any treatment plan.
Interested in more advice from ob/gyns? Keep reading!
Gynecologists Break the Silence On 'Hair Down There' Over 50 — All Your Questions Answered
Are Your Menopausal Nipple Changes Normal? Here's What an Ob/Gyn Wants You To Know
View comments




Comments
Post a Comment