Secnidazole Offers Hope as Option for Treating Trichomoniasis in Women - Contagionlive.com
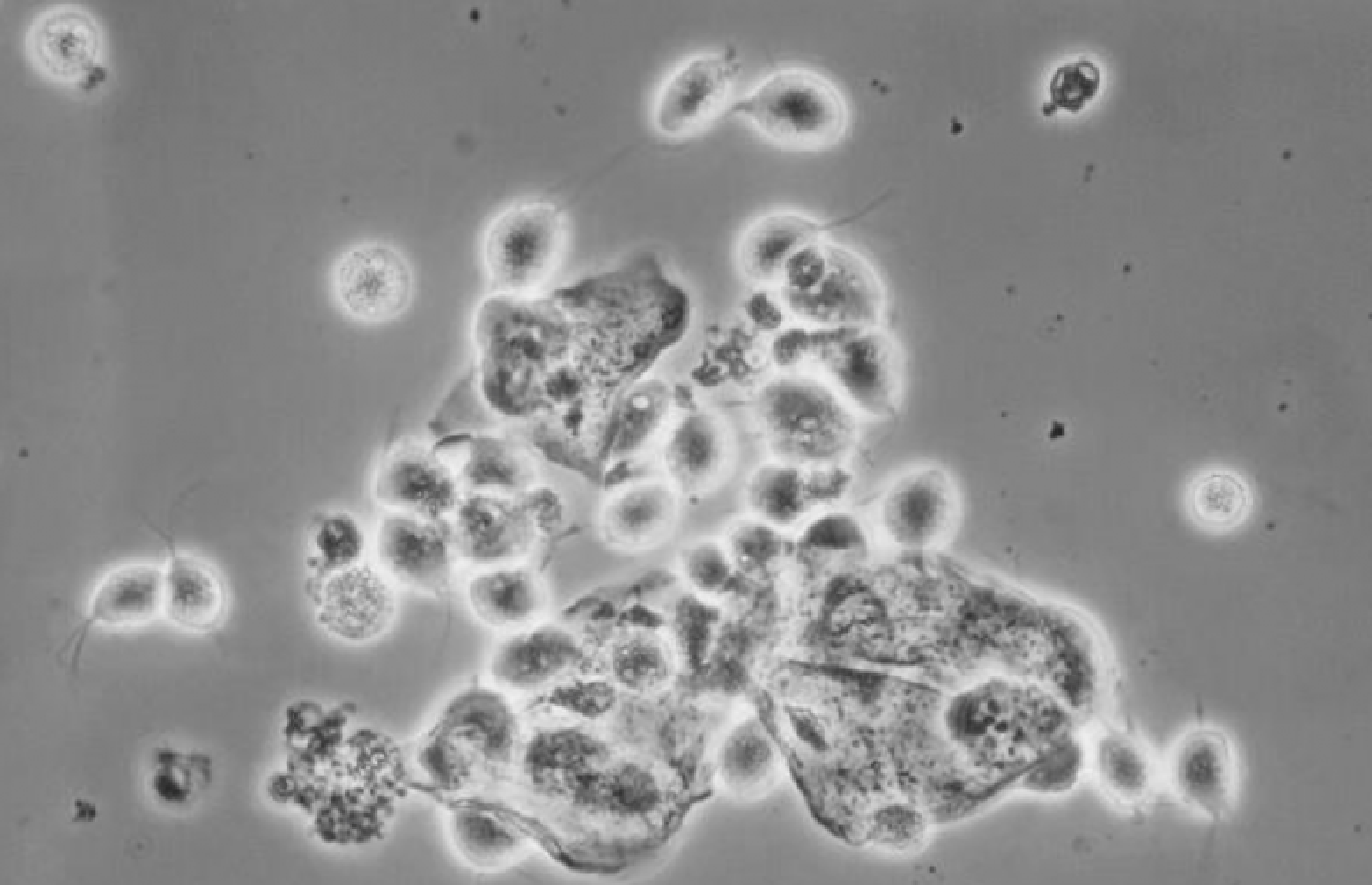
Trichomonas vaginalis is a protozoan parasite estimated to affect 3.7 million individuals in the United States, including 2.1% of women aged 14 to 59 years. Black women are disproportionately affected, with an increased prevalence rate of 9.6%.1,2 Potential complications of trichomoniasis include increased risk of other sexually transmitted infections (STIs) including HIV and adverse birth outcomes in pregnancy.2,3
Previously, the recommended treatment for trichomoniasis in HIV-uninfected individuals was a single oral dose of metronidazole. However, a recent randomized controlled trial reported that a 7-day course of metronidazole resulted in 45% fewer treatment failures compared with the single dose (10.9% vs 18.6%; relative risk [RR], 0.55; 95% CI, 0.34-0.70).4 In the 2021 US Centers for Disease Control and Prevention (CDC) STI guidelines, the recommended trichomoniasis treatment regimen was revised to 7 days of metronidazole for all women.
Secnidazole is a nitroimidazole antibiotic with a prolonged half-life of 17 hours, compared with 7 to 8 hours for metronidazole and 12 hours for tinidazole. It was initially approved by the FDA in 2017 for bacterial vaginosis (BV) and is included as an alternative agent and the only single-dose regimen for BV treatment.2 Literature from other countries in the 1970s and 1980s described clinical efficacy of a single dose of secnidazole for treatment of trichomoniasis with parasite eradication rates greater than 90%.5 In June 2021, with the results of this phase 3 trial (NCT03935217), secnidazole received FDA approval for the additional indication of trichomoniasis treatment.
Muzny et al conducted this randomized, double-blind, placebo-controlled, delayed treatment study in postmenarchal females (12 years and older) diagnosed with T vaginalis infection. Patients who were pregnant or lactating, had symptomatic vulvovaginal candidiasis, or received antimicrobial treatment in the previous 14 days were excluded. Patients were randomized 1:1 to receive a single dose of secnidazole 2 g oral granules or matching placebo that was taken under direct observation at visit 1. Visit 2 occurred 6 to 12 days later to assess test-of-cure and treatment-emergent adverse events (TEAEs). Patients also received the opposite treatment at this time. For patients not meeting test-of-cure criteria, third and fourth visits were scheduled for additional treatment.
The primary efficacy end point was microbiological cure with the InPouch culture device at the test-of-cure visit in the modified intention-to-treat (mITT) population, defined as patients with a positive T vaginalis culture and negative chlamydia and gonorrhea testing at baseline. The analysis was adjusted for presence of trichomoniasis symptoms.
The study enrolled 147 women; 131 were included in the mITT population. More than 90% of patients included were Black/African American. Of note, 29% of patients had BV coinfection and 6.9% were HIV positive. Microbiological cure at test-of-cure was achieved in 92.2% (95% CI, 82.70%-97.41%) of the secnidazole group compared with 1.5% (95% CI, 0.04%-8.04%) of the placebo group (P < .001). Post hoc subgroup analyses in patients with symptoms, without symptoms, BV coinfection, and HIV infection suggested similar results (Table).
TEAEs were assessed in the safety population of all patients who received at least 1 dose of study medication. Overall, the rates of reported AEs were lower in the secnidazole group compared with placebo (14.9% vs 21.9%) and included nausea, diarrhea, headache, and vulvovaginal candidiasis. All reported events were mild and no serious events occurred.
Secnidazole was found to be efficacious for treatment of trichomoniasis in women and was generally well tolerated. Efficacy seemed to be maintained in patients with BV coinfection and in patients with HIV infection; however, larger confirmatory studies are needed for these populations. As an additional single-dose option for trichomoniasis treatment, secnidazole may be advantageous for patients with difficulty adhering to a 7-day metronidazole course. However, with tinidazole as a guideline-recommended single-dose treatment for trichomoniasis and the lack of head-to-head comparative trials, cost-effectiveness will impact secnidazole's place in therapy. Furthermore, although animal studies did not find adverse developmental outcomes with secnidazole use in pregnancy,6 metronidazole remains the preferred treatment in pregnancy due to a paucity of clinical safety data with tinidazole and secnidazole. One notable advantage of secnidazole over the other nitroimidazoles is that it is the only single-dose treatment regimen for BV. The prevalence of trichomoniasis and BV coinfection was 29% in the present study and has been reported to be as high as 60% to 80% in the literature.7 Prior to secnidazole's approval, treatment of these patients was limited to multidose regimens with either metronidazole or tinidazole, representing a group that may benefit most from a 2-for-1 single-dose treatment option.
References
- Flagg EW, Meites E, Phillips C, Papp J, Torrone EA. Prevalence of Trichomonas vaginalis among civilian, noninstitutionalized male and female population aged 14 to 59 years: United States, 2013 to 2016. Sex Transm Dis. 2019;46(10):e93-e96. doi:10.1097/OLQ.0000000000001013
- Workowski KA, Bachmann LH, Chan PA, et al. Sexually transmitted infections treatment guidelines, 2021. MMWR Recomm Rep. 2021;70(4):1-187. doi:10.15585/mmwr.rr7004a1
- McClelland RS, Sangare L, Hassan WM, et al. Infection with Trichomonas vaginalis increases the risk of HIV-1 acquisition. J Infect Dis. 2007;195(5):698-702. doi:10.1086/511278
- Kissinger P, Muzny CA, Mena LA, et al. Single-dose versus 7-day-dose metronidazole for the treatment of trichomoniasis in women: an open-label, randomised controlled trial. Lancet Infect Dis. 2018;18(11):1251-1259. doi:10.1016/S1473-3099(18)30423-7
- Gillis JC, Wiseman LR. Secnidazole. A review of its antimicrobial activity, pharmacokinetic properties and therapeutic use in the management of protozoal infections and bacterial vaginosis. Drugs. 1996;51(4):621-638. doi:10.2165/00003495-199651040-00007
- Solosec (secnidazole). Product information. Lupin Pharmaceuticals; 2021.
- Sobel JD, Subramanian C, Foxman B, Fairfax M, Gygax SE. Mixed vaginitis-more than coinfection and with therapeutic implications. Curr Infect Dis Rep. 2013;15(2):104-108.doi:10.1007/s11908-013-0325-5


Comments
Post a Comment