Juggling Medications, Lab Tests, and Side Effects After Transplant - Pulmonary Fibrosis News
My pulmonologists are talented jugglers. They must determine my medication dosages, keep my lab results within the standard ranges, and minimize medication side effects. After my bilateral lung transplant in August 2020, it took a year to find the correct balance between all three.
Medication baseline
The balancing act started right after the surgery. Pulmonologists begin with a standard list of drugs, then modify it for each patient. By the time I was discharged from the hospital post-transplant, my team had developed a list of drugs I could take for my existing health issues. It was significantly different from what I had taken pre-transplant, but it covered all my medical conditions. The changes are noted in the following table:
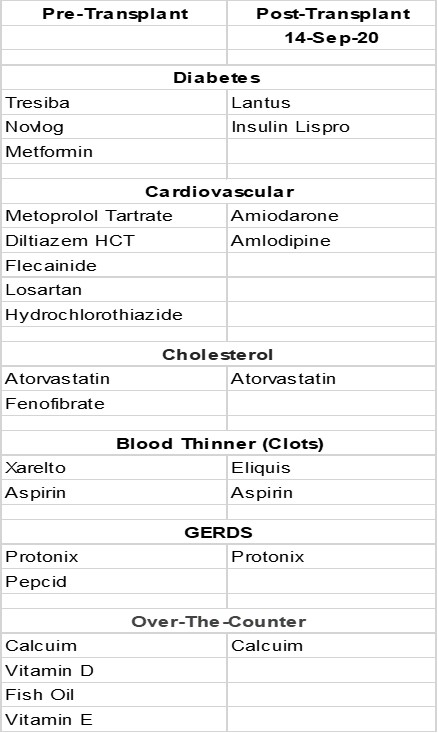
Kevin's medications pre- and post-transplant. (Courtesy of Kevin Olson)
The transplant itself required me to start six additional medications. The immunosuppressants included prednisone, CellCept (mycophenolate mofetil), and Prograf (tacrolimus). I will take these anti-rejection meds for life. The anti-infection medications included Mepron (atovaquone), Valcyte (valganciclovir), and Diflucan (fluconazole).
Mepron is an antibiotic that prevents and treats Pneumocystis jiroveci pneumonia, a serious lung infection. I will be on it for life. Valcyte is an antiviral that prevents and treats cytomegalovirus (CMV) infection. It was eventually replaced with acyclovir, another antiviral. Diflucan is an antifungal that prevents and treats fungal infections. I took it for six months after transplant.
I'm currently on 15 medications, and can't imagine the number of possible interactions. Several interactions influenced my lab results, which dictated multiple changes in dosages and meds.

Juggling act No. 1
One of the risks of taking CellCept is developing viral infections such as CMV. I started at 2,000 mg a day, but developed a mild CMV infection. The treatment was to increase my Valcyte dosage and stop taking CellCept.
Once the CMV infection was gone, the pulmonologists restarted me on a low dose of CellCept and decreased my Valcyte dosage. They began to steadily increase my CellCept dosage, but once again, a CMV infection struck before I had reached 2,000 mg. Again, the CellCept was stopped and the Valcyte was increased.
After the infection was gone, my Valcyte was replaced with acyclovir. Additionally, my CellCept was restarted, but my issues with CMV returned, and the cycle began again.
This continued for a year until I was permanently placed on 500 mg of CellCept and prescribed Valcyte for an additional six months.
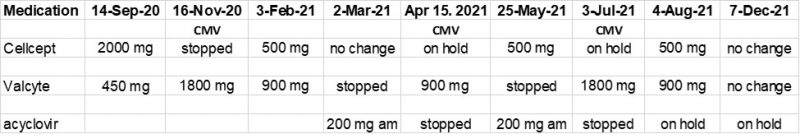
Kevin's cycle of med changes due to CMV infections. (Courtesy of Kevin Olson)
Juggling act No. 2
My pulmonologists continuously monitored the amount of tacrolimus in my blood. For me, a standard range of concentration is 5-9 ng/mL, and anything below or above that requires a change in dosage.
In the beginning, my levels would change twice a week, but over time, they only changed about once a week. Once again, it took a year to arrive at a semi-permanent dose. I thought my veins would dry up from all the blood draws.
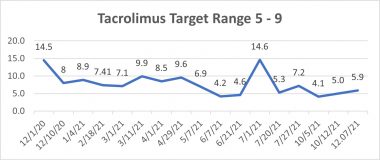
Kevin's lab results show the concentration of tacrolimus in his blood. (Courtesy of Kevin Olson)
Juggling act No. 3
As my body absorbed all these medications, I experienced several side effects, and some of my lab results went outside the standard range.
Side effects could include:
- Increased blood pressure and blood sugar
- Nausea and vomiting
- Decreased white blood cell and platelet count
These effects and the nonstandard lab results were a recipe for more medication.
The pulmonologist changed my blood pressure meds to carvedilol and olmesartan, and added ferrous sulfate (iron), vitamin C, and vitamin D. Now, I was taking a measly 17 medications and vitamins.
Managing my medications
I have become a juggler, too. At first glance, my medication management felt like an insurmountable task.
The hospital pharmacist required me to know the name and purpose of each immunosuppressant and anti-infection medication. Then, the nurses started teaching me the names and reasons behind all of my other medications. When I was discharged after transplant, I passed the pharmacist's quiz.
Once I was home, I was responsible for organizing my meds. I continued using pillboxes, as I had done pre-transplant. The pharmacist provided a medication list that included the dosages and time of day for each. It helped me fill my pillboxes correctly.
Early on, dosages changed every week, and I had to modify my pillboxes. It was challenging. Additionally, I kept a lung transplant log where I noted each dosage change. The log kept me straight about the number of pills required.
After a year, my dosages were stable, and drug administration was significantly more manageable. But the most critical part for me was that the frequency of my blood draws decreased from once a week to once every two months. This has improved my quality of life.
***
Note: Pulmonary Fibrosis News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The opinions expressed in this column are not those of Pulmonary Fibrosis News or its parent company, BioNews, and are intended to spark discussion about issues pertaining to pulmonary fibrosis.


Comments
Post a Comment